


Public health safety in India has been greatly challenged due to COVID-19. More organized infection prevention and control have become of prime importance to safeguard the interest of the patients as well as the dentists.
The dental professionals are the most threatened groups during the ongoing COVID-19 crisis due to close contact with patients, exposure to bodily fluids, and the handling of sharp instruments.
So what can you do to keep yourself, your dental practice, and your patients safe? Indian Dental Association (IDA) and Oral B have launched the ‘Smile Suraksha Programme’ – an online learning platform to empower our member dentists with a list of procedures that make you, your dental office, and patients safe.
Guidelines for dental care provision during the COVID-19 pandemic are developed after considering the nature of COVID-19 pandemic, and grouping the patients according to condition and need, and considering the procedures according to risk and benefit. These guidelines include advice to dentists on being diligent and to follow strict screening measures and stringent infection control prevention protocols, standard protocols of patient management which ensure your patients and staff members ease of mind during dental visits and procedures.
All members are requested to study the online SOPs upon completion of which the members will receive certification under the ‘Smile Suraksha Programme’ along with safety and precaution posters, which can be displayed in the clinic to bring reassurance to patients that dental care is delivered in a ‘safe’ environment.
IDA and Oral B are committed to practicing safe dentistry for dentists, patients, and the community.
The new variant of the coronavirus which caused SARS, but now in a mutated, highly contagious version is called NOVEL CORONAVIRUS 2019, and the disease is called COVID-19.
Potentially life threatening and require urgent and immediate treatment to stop ongoing tissue bleeding, alleviate severe pain or infection which includes the following:-
According to the CDC guidelines, not everyone needs to be tested for COVID-19, which includes dentists. It also suggests that the decision on who is to be tested is at the discretion of local and state health departments and individual clinics. ICMR guidelines also suggest in their revised testing strategy, dated 20/3/2020, that the following people need to be tested:
If the dentist and the clinical staff do not fall in these categories, getting tested for COVID-19 is not warranted. However, as suggested by CDC, it is at the discretion of the individual clinics. Also, since majority of clinical staff in the Indian context do not have health professional background and carry the risk of exposure from neighborhoods, it would be a wise idea to follow ‘Tele-screening and Triaging’ for clinical staff by conducting initial telephone screening using the screening questionnaire suggested for patients, before they resume their duties in the clinics.
For patients, initial screening for symptoms should be done as a part of care provision, which is not only a risk reduction strategy but also boosts the confidence of the patients in availing care. If the clinician chooses to get the patients tested for COVID-19, tests may be sent to the private labs to avoid the burden on the state-run hospitals and labs. If the management of the clinic chooses to get the staff and consultants tested as a risk reduction strategy, it is advisable that the expenses are arranged for by the management.
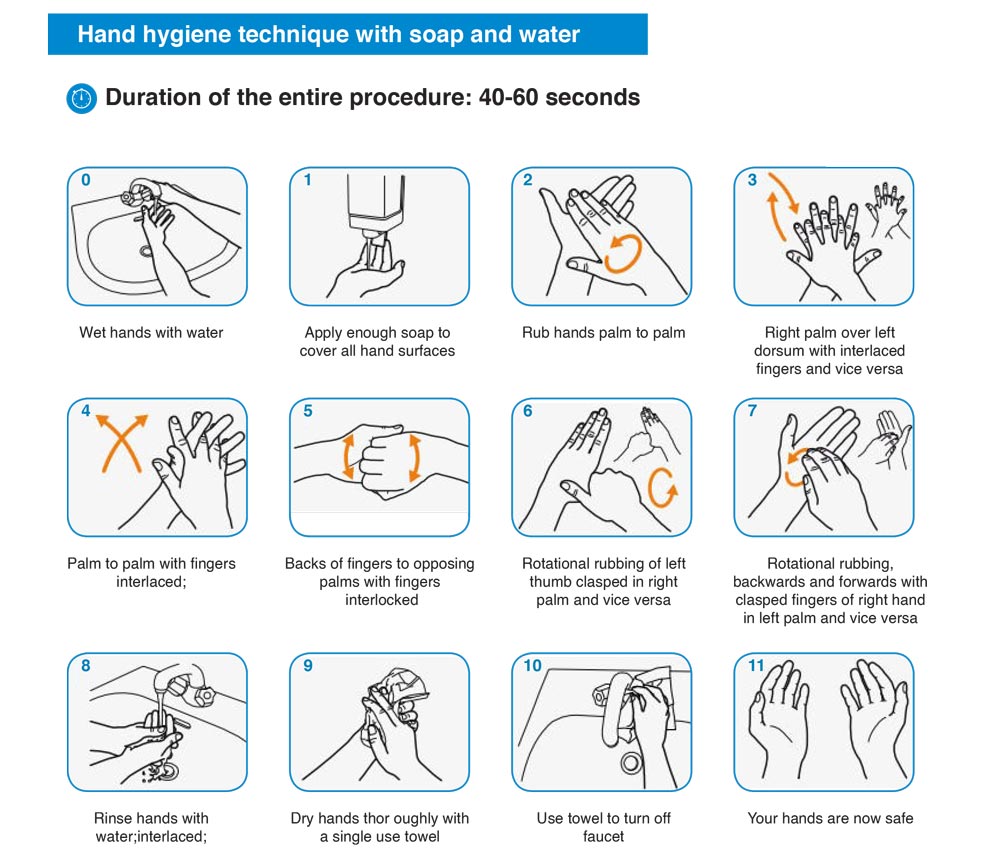
Hand hygiene should be practiced at the following key stages in the decontamination process so as to minimise the risk of contamination:

The current global stockpile of PPE is insufficient, particularly for medical masks and respirators; the supply of gowns and goggles is soon expected to be inadequate also. Surging global demand-driven not only by the number of COVID-19 cases but also by misinformation, panic buying, and stockpiling − will result in further shortages of PPE globally. The capacity to expand PPE production is limited, and the current demand for respirators and masks cannot be met, especially if widespread inappropriate use of PPE continues.48
If basic PPE, including surgical facemasks are not available, do not proceed with any dental procedure, regardless of emergency/urgent patients.
48.jpg)
As dental treatments fall under high-risk category for airborne and droplet infections such as COVID-19 strict measures have to be followed to ensure operator and patient safety
The use of personal protective equipment, including masks, gloves, gowns, and goggles or face shields, is recommended to protect skin and mucosa from (potentially) infected blood or secretion. As respiratory droplets are the main route of SARS-CoV-2 transmission, particulate respirators (e.g., N-95 masks authenticated by the National Institute for Occupational Safety and Health or FFP2-standard masks set by the European Union) are recommended for the routine dental practice.
Recommended personal PPE during the outbreak of COVID-19 outbreak, according to the setting, personnel, and type of activity.
Display charts or guidelines proposed by CDC or WHO for wearing and removing PPEs in their designated areas.
https://www.who.int/csr/resources/publications/PPE_EN_A1sl.pdf ,
Properly train your staff to adhere to the above-said principles
| Setting | Target personnel or patients | Activity | Type of PPE or procedure |
|---|---|---|---|
| Health care facilities - Inpatient facilities | |||
| Patient room | Health care workers | Providing direct care to COVID-19 patients |
Medical mask Gown Gloves Eye protection (goggles or face shield) |
| Aerosol-generating procedures performed on COVID-19 patients |
Respirator N95 or FFP2
standard, or equivalent.
Gown Gloves Eye protection Apron |
||
| Cleaners | Entering the room of COVID-19 Patients |
Medical mask Gown Heavy-duty gloves Eye protection (if risk of splash from organic material or chemicals) Boots or closed work shoes |
|
| Visitors | Entering the room of a COVID- 19 patient |
Medical mask Gown Gloves |
|
| Other areas of patient transit (e.g. wards, corridors). | All staff, including health care workers | Any activity that does not involve contact with COVID-19 patients | No PPE required |
| Triage | Health care workers | Preliminary screening not involving direct contact | Maintain spatial distance of at least 1 metre. No PPE required |
| Patients with respiratory symptoms | Any | Maintain spatial distance of at least 1 metre. Provide medical mask if tolerated by patient. | |
| Patients without respiratory symptoms | Any | No PPE required | |
| Laboratory | Lab technician | Manipulation of respiratory Samples |
Medical mask Gown Gloves Eye protection (if risk of splash) |
| Administrative areas | All staff, including health care workers. | Administrative tasks that do not involve contact with COVID-19 patients. | No PPE required |
| Health care facilities - Outpatient facilities | |||
| Consultation room | Health care workers | Physical examination of patient with respiratory symptoms |
Medical mask Gown Gloves Eye protection |
| Health care workers | Physical examination of patients without respiratory symptoms | PPE according to standard precautions and risk assessment. | |
| Patients with respiratory symptoms | Any | Provide medical mask if tolerated | |
| Patients with respiratory symptoms | Any | No PPE required | |
| Cleaners | After and between consultations with patients with respiratory symptoms. |
Medical mask Gown Heavy-duty gloves Eye protection (if the risk of splash from organic material or chemicals). Boots or closed work shoes |
|
| Waiting room | Patients with respiratory symptoms | Any | Provide medical mask if tolerated. Immediately move the patient to an isolation room or separate area away from others; if this is not feasible, ensure the spatial distance of at least 1 meter from other patients. |
| Patients without respiratory symptoms | Any | No PPE required | |
| Administrative areas | All staff, including health care workers | Administrative tasks | No PPE required |
| Triage | Health care workers | Preliminary screening not involving direct contact | Maintain a spatial distance of at least 1 meter. No PPE required |
| Patients with respiratory symptoms | Any | Maintain a spatial distance of at least 1 meter. Provide medical mask if tolerated by the patient. | |
| Patients without respiratory symptoms | Any | No PPE required | |
Checklist for isolation room or area trolley or table
The following items should be kept on the trolley at all times so that PPE is always available for healthcare workers.
| S.No | Equipment | Stock Present |
|---|---|---|
| 1 | Eye protection (visor or goggles) | |
| 2 | Face shield (provides eye, nose and mouth protection) | |
| 3 |
Gloves
|
|
| 4 | Hair covers (optional) | |
| 5 | Particulate respirators (N95, FFP2, or equivalent) | |
| 6 | Medical (surgical or procedure) masks | |
| 7 |
Gowns and aprons
|
|
| 8 | Alcohol-based hand rub | |
| 9 | Plain soap (liquid if possible, for washing hands in clean water) | |
| 10 | Clean single-use towels (e.g. paper towels) | |
| 11 | Sharps containers | |
| 12 | Appropriate detergent for environmental cleaning and disinfectant for disinfection of surfaces, instruments or equipment | |
| 13 | Large plastic bags | |
| 14 | Appropriate clinical waste bags | |
| 15 | Linen bags | |
| 16 | Collection container for used equipment |
Postoperative instructions for patients- it is recommended that NSAIDS in combination with acetaminophen can still be used for management of pulpal and periapical related dental pain and intraoral swelling
https://www.sciencealert.com/who-recommends-to-avoid-taking-ibuprofen-for-covid-19-symptomsIn all restrictions, urgent dental treatment for people who have been identified as either at moderate to high risk of COVID-19 or confirmed as COVID-19 case should be provided under transmission based on precautions using appropriate PPE
| Services that can be performed | Restricted services / defer treatment | |
|---|---|---|
| No Restrictions | All dental services | No restrictions apply |
| Level 1 Restrictions | All dental treatment using standard precautions for people who do not meet epidemiological or clinical risk factor for COVID-19 infection transmission |
Defer non-urgent treatment for people who DO meet epidemiological or clinical symptom criteria for COVID-19 risk. Urgent dental treatment for people who DO meet epidemiological or clinical symptom criteria for COVID-19 risk or confirmed as COVID-19 case |
| Level 2 Restriction |
Provision for dental treatments that are unlikely to generate aerosols or where aerosols generated have the presence of minimal saliva / blood due to use of rubber dam. This includes
|
Defer all treatment that likely to be generating aerosols which may include the use of
All surgical extractions should be referred to specialist oral surgeon who will undertake these procedures using transmission based precautions. Elective implant treatment should be delayed. Urgent dental treatment for people who DO meet epidemiological or clinical symptom criteria for COVID-19 risk or confirmed as a COVID-19 case, |
| Level 3 Restriction |
Only dental treatments that do not generate aerosols, or where treatments generating aerosols is limited to:
|
Defer all routine recall examinations and dental treatments for patients not fitting the risk categories identified in the left who present with the following concerns
Urgent dental treatment for people who DO meet epidemiological or clinical symptom criteria for COVID-19 risk or confirmed as a COVID-19 case |
| Level 4 Restriction |
Only the following dental treatment to be managed:
|
Defer all dental treatments for patients not fitting the risk categories identified on the left. Urgent dental treatment for people who DO meet epidemiological or clinical symptom criteria for COVID-19 risk or confirmed as a COVID-19 case, |
| Level 5 Restriction | No routine dental treatment provided. All patients with acute dental concerns to be directed to emergency care centres. | Any dental treatment without expressed permission from the public health authorities. |
Keeping all staff protected from chronic stress and poor mental health during this response means that they will have a better capacity to fulfill their roles. Be sure to keep in mind that the current situation will not go away overnight and you should focus on longer-term occupational capacity rather than repeated short-term crisis responses. Ensure that good quality communication and accurate information updates are provided to all staff. Rotate workers and partner inexperienced workers with their more experienced colleagues. The buddy system helps to provide support, monitor stress and reinforce safety procedures. Support all staff in taking care of themselves at this time. Encourage them to use helpful coping strategies such as:
Encourage staff to avoid using unhelpful coping strategies such as:
The COVID-19 outbreak is a unique and unprecedented scenario for many workers. Prepare them mentally as this is not a sprint; it’s a marathon. Provide clinical staff with refresher training in infection prevention and control.
Treat waste contaminated with blood, body fluids, secretions and excretions as clinical waste, in accordance with local regulations. Human tissues and laboratory waste that is directly associated with specimen processing should also be treated as clinical waste.
Discard single use items properly
Visual alerts posters issued by CDC can be accessed here:
https://www.cdc.gov/flu/pdf/protect/cdc_cough.pdf
https://www.cdc.gov/coronavirus/2019-ncov/downloads/stop-the-spread-of-germs.pdf
https://www.cdc.gov/coronavirus/2019-ncov/php/risk-assessment.html
Telehealth refers to a broad variety of technologies and tactics to deliver virtual medical, health, and education services. Telehealth is not a specific service, but a collection of means to enhance care and education delivery. Teledentistry refers to the use of telehealth systems and methodologies in dentistry. Teledentistry can include patient care delivery using, but not limited to, the following modalities:
During this pandemic our goal as dental care providers is to use telecommunication technology to triage patients and conduct problem-focused evaluations to limit office visits to urgent or emergency care. This can facilitate providing advice and performing triage. It can also facilitate planning for in-person interactions should they become necessary.
Contacts…
https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html
[accessed on 9th April, 2020]https://www.mohfw.gov.in/pdf/GuidelinesonClinicalManagementofCOVID1912020.pdf
[accessed on 6th April, 2020]https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/testing.html
[accessed on 6th April, 2020]https://icmr.nic.in/sites/default/files/upload_documents/2020-03-20_covid19_test_v3.pdf
[accessed on 6th April, 2020]https://www.ada.org/~/media/CPS/Files/COVID/ADA_Int_Guidance_Mgmt_Emerg-Urg_Dental_COVID19.pdf
http://apps.who.int/iris/bitstream/10665/112656/1/9789241507134_eng.pdf?ua=1
https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf
[accessed on 9th April, 2020].https://success.ada.org/~/media/CPS/Files/COVID/ADA_COVID_Coding_and_Billing_Guidance.pdf
Ministry of Health and Family Welfare Directorate General of Health Services [ Emergency Medical Relief ]
Novel Coronavirus Disease 2019 (COVID-19): Additional guidelines on rational use of Personal Protective Equipment (setting approach for Health functionaries working in Non-COVID areas)
This guideline is for health care workers and others working in Non-COVID hospitals and Non-COVID treatment areas of a hospital which has a COVID block. These guidelines are in continuation of guidelines issued previously on ‘Rational use of Personal Protective Equipment’
( https://www.mohfw.gov.in/pdf/GuidelinesonrationaluseofPersonalProtectiveEquipment.pdf ).
This guideline uses “settings” approach to guide on the type of personal protective equipment to be used in different settings.| S.No | Setting | Activity | Risk | Recommended PPE | Remarks |
|---|---|---|---|---|---|
| 1 | Help desk/ Registration counter | Provide information to patients | Mild risk |
|
Physical distancing to be followed at all times |
| 2 | Doctors chamber | Clinical management | Mild risk |
|
"No aerosol generating procedures should be allowed." |
| 3 | Chamber of Dental/ ENT doctors/ Ophthalmology doctors | Clinical management | Moderate risk |
|
Aerosol generating
procedures anticipated. Face shield, when a splash of body fluid is expected |
| 4 | Pre- anesthetic check-up clinic | Pre-anesthetic check-up | Moderate risk |
|
* Only recommended when close examination of oral cavity/dentures is to be done |
| 5 | Pharmacy counter | Distribution of drugs | Mild risk |
|
Frequent use of hand sanitizer is advised over gloves. |
| 6 | Sanitary staff | Cleaning frequently touched surfaces/ Floor | Mild risk |
|
#All hospitals should identify a separate triage and holding area for patients with Influenza like illness so that suspect COVID cases are triaged and managed away from the main outpatient department.
| S.No | Setting | Activity | Risk | Recommended PPE | Remarks |
|---|---|---|---|---|---|
| 1 | Ward/ individual rooms | Clinical management | Mild risk |
|
Patients stable. No aerosol generating activity |
| 2 | ICU/ Critical care | Critical care management | Moderate risk |
|
Aerosol generating
activities performed. Face shield, when a splash of body fluid is expected |
| 3 | Ward/ICU /critical care | Dead body packing | Low Risk |
|
|
| 4 | Ward/ICU/ Critical care (Non-COVID) | Dead body transport to mortuary | Low Risk |
|
|
| 5 | Labor room | Intra-partum care | Moderate Risk |
|
Patient to be masked in the Labor room *If the pregnant woman is a resident of containment zone |
| 6 | Operation Theater | Performing surgery, administering general anaesthesia | Moderate Risk |
|
Already OT staff shall be wearing For personnel involved in aerosol generating procedures |
| 7 | Sanitation | Cleaning frequently touched surfaces/ floor/ changing linen | Low Risk |
|
| S.No | Setting | Activity | Risk | Recommended PPE | Remarks |
|---|---|---|---|---|---|
| 1 | Emergency | Attending emergency cases | Mild risk |
|
No aerosol generating procedures are allowed |
| 2 | Attending to severely ill patients while performing aerosol generating procedure | High risk | Full complement of PPE (N-95 mask, coverall, goggle, Nitrile examination gloves, shoe cover) |
| S.No | Setting | Activity | Risk | Recommended PPE | Remarks |
|---|---|---|---|---|---|
| 1 | Routine Laboratory | Sample collection and transportation and testing of routine (non- respiratory) samples | Mild risk |
|
|
| Respiratory samples | Moderate risk |
|
|||
| 2 | Radio-diagnosis, Blood bank, etc. | Imaging services, blood bank services etc | Mild risk |
|
|
| 3 | CSSD/Laundry | Handling linen | Mild risk |
|
|
| 4 | Other supportive services incl. Kitchen | Administrative Financial Engineering** and dietary** services,etc. | Low risk | Face cover | ** Engineering and dietary service personnel visiting treatment areas will wear personal protective gears appropriate to that area |
| S.No | Setting | Activity | Risk | Recommended PPE | Remarks |
|---|---|---|---|---|---|
| 1 | Ambulance Transfer to designated hospital | Transporting patients not on any assisted ventilation | Low risk |
|
|
| Management of SARI patient | High risk | Full complement of PPE (N-95 mask, coverall, goggle, latex examination gloves, shoe cover) | While performing aerosol generating procedure | ||
| 2 | Driving the ambulance | Low risk |
|
Driver helps in shifting patients to the emergency |
In addition, patients and their attendants to be encouraged to put on face cover.
In case a COVID-19 patient is detected in such Non-COVID Health facility, the MoHFW guidelines for the same has to be followed
(Available at:https://www.mohfw.gov.in/pdf/GuidelinestobefollowedondetectionofsuspectorconfirmedCOVID19case.pdf)

